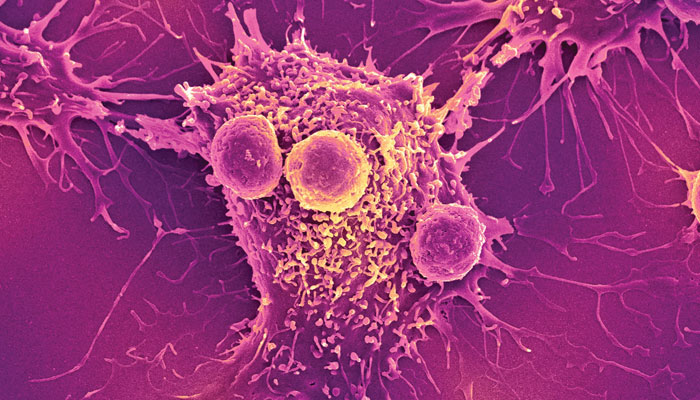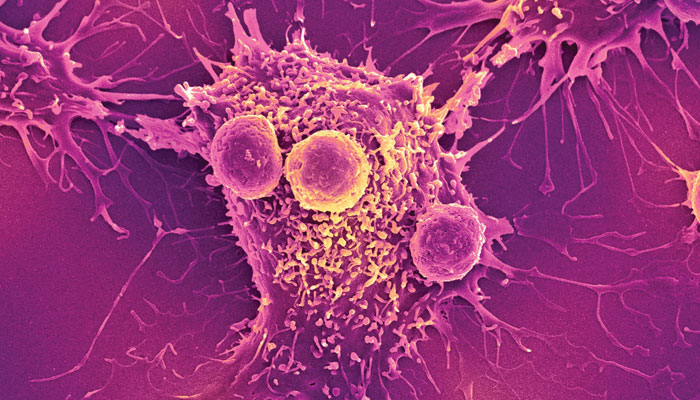
Medical experts are introducing new methods, stem cell therapies and therapies to treat malignant diseases like cancer. Details of some of them are given below.
Shock treatment for cancer
When nanosecond high voltage pulses are applied to cancer cells, these cells self-destruct. This method can be used to treat cancer. These nanosecond pulses have a longer-lasting effect than the microsecond pulses used in laser guns, which wear off much faster.
The silkworm and the dragonfly… gene therapy
The spider is undoubtedly an amazing creature. So far, there are 400,000 species of spiders in human knowledge. The thread that the silk spider makes is stronger than steel in terms of weight. The glue that holds the spider web together contains two types of proteins that have evolved over thousands of years to have this strength. Jugnu is another surprising insect. Have you seen Jagno shining at night? The reason for this is a special protein in them, luciferase, which produces energy in the form of light by chemically interacting with a substance called luciferin.
Tufts University Professor David Kaplan and his colleagues have modified the silk thread and combined it with a gene protein to treat breast cancer through gene therapy. Gene therapy or gene therapy for certain diseases. Treatment is a method of correcting a gene defect (by modifying the defective gene and inserting a functional gene into the genome). The scientists inserted a gene into the silkworm to modify its genetic makeup and then attached it to the diseased cells.
As a result of this process, the same protein is produced which is responsible for the glow of the lamp at night. A genetically modified silkworm protein selectively binds to cancer cells in breast cancer patients and causes the cells to glow. Through this, these cells are easily identified in cancer patients.
Stem cells… missiles in the war against cancer
Stem cell research is opening new avenues for the treatment of heart, kidney and other diseases. Now stem cells are being used as a guard missile for cancer treatment. A team of scientists at the Duarte Beckmann Research Institute in Duarte, California, injected genetically modified stem cells into the brains of mice with brain cancer and then gave the mice anti-cancer drugs. Gone. (5-Fluorouracil).
It was found that mice that were first treated with stem cells had a 70 percent reduction in tumor size compared to untreated mice, but also prevented the secondary growth of these cells. Yes, by following this method even a single cancer cell can be targeted. Human experiments using this concept will be started soon.
Stem cells… new frontiers in medicine
A new emerging field in the field of medicine is the use of stem cells to repair damaged organs. There are two types of stem cells used in humans. Embryonic stem cells and adult stem cells. Stem cells work together with other cells to repair damaged tissues in the body, as they have the ability to differentiate into different types of cells in the body. By growing these cells in culture, they can be transformed into different types of cells, such as neural, inflammatory or intestinal cells.
A recent breakthrough in stem cell research has shown that different types of stem cell release from bone marrow can be induced by infiltration with different drugs. However, instead of using stem cells obtained from different donors (in which case the patient’s body may refuse to accept those stem cells), the patient’s own stem cells are removed from the bone marrow. If done, it can help in the repair and regeneration of specific tissues.
The ability to selectively remove a patient’s own stem cells is a critical advance in this rapidly developing field. The work was carried out by Professor Sarah Rankin of Imperial College London and her colleagues. This development will help speed up the repair of damaged heart tissue and the repair of broken bones and joints.
A new approach to cancer treatment
According to a study, 31 percent of deaths in the world are caused by cancer. Efforts are being made to treat various types of cancer, some of which have achieved significant success. One way to treat cancer is to deliver drugs directly to cancer cells, so that other healthy cells in the body are protected from the toxic effects of these drugs.
Mark Ostermen, Johns Hopkins Professor of Chemical and Biomolecular Engineering at the Whiting School of Engineering, and Ames R. Etshman, Professor of Geology and Oncology at the Johns Hopkins School of Medicine, are investigating how cancer cells themselves develop their therapeutic potential. Be done.
In this way, cancer cells will destroy themselves without harming other healthy cells. Under this theory, a “Protein Switch” will be prepared by combining two different proteins. One of these proteins will recognize the cancer cells and the other will have the ability to convert the inactive prodrug into a substance that is lethal to the cancer. In the first step, the “switch” will be inserted into the cancer cells, then the patient will be given an inactive prodrug. When this prodrug approaches the cancer cells, the protein will recognize the cancer cells and convert the inactive prodrug into the active drug, which will then kill the cancer cells.
A New Cancer Treatment … From a River of Light (Plasmons)
Another new cancer treatment method is in development. In this, light waves are made to travel along a predetermined path. Oscillation, or plasmons, can be compared to the process of throwing a stone into a still pool of water, which creates ripples on the surface of the water. Similarly, if light particles (photons) hit a metal, the vibration caused by the electron spreads across the surface, carrying more light with it.
Thus rivers of light are created. The search for the application of plasmons in various fields of science continues, including cancer treatment, solar cells and visual computing, biochemical sensitivity, bio chemical sensing. For this reason, it has become an important part of the field of physics. Nomani Halas of Rice University in Houston mixed gold nanoparticles with cancer-fighting antibodies and injected them into the body of mice.
As the nano-particle antibody unit binds to the tumor, the tumor is exposed to weak infrared light, which is then destroyed by the nano-particles. This method of treating cancer has shown great results in mice and is now being tested more closely in humans. Many types of cancer are treated by exposing them to “rivers of light,” which travel on electron waves.
Early diagnosis of cancer…dramatic progression
According to the report, every year 8 lakh people die due to cancer. The main problem with this disease is that it is detected when it has grown enough, in lung cancer, the tumor is seen when it is about the size of a cricket ball. However, 9 percent of lung cancer patients die within five years of diagnosis.
Routine health screening makes it difficult to detect early cancer, making late diagnosis of the disease so difficult to treat. (UK Nottingham) and Kansas ( After 51 years of research, scientists and doctors of the United States have developed a simple blood test for the diagnosis of cancer, which is being called an important milestone in the diagnosis of this disease. This new technology involves tracking the first molecular sign of cancer. When cancer cells begin to form, certain proteins (antigens) are produced that stimulate the body’s immune system and respond by forming antibodies. .
A blood test developed will detect this activity and help scientists identify the exact antigens and antibodies that bind to them, thereby identifying the type of cancer tumor that is forming. This work will be done with just 10 ml of blood from the patient which will be included in the routine test through which the cancer will be detected in the early stage which is usually a curable stage. This test is being conducted in America and Britain. The test has shown dramatic improvements in the treatment of lung cancer patients in pilot studies and significant improvements in 9% of other solid cancers.
Cancer… predicting its spread
Cancer accounts for 31% of all deaths each year. This rate continues to increase as the average age increases and the elderly population increases. With the development of new drugs, cancer has now become a curable disease. Especially if it is detected at an early stage, most tumors are prone to secondary growth (metastasis), which is fatal.
However, efforts are now being made to detect this type of growth trend in the beginning before they occur. In Bethesda, Maryland, USA, the National Institute of Health and Human Development has achieved significant success in this regard. has come
They have found that before secondary growth occurs, a modified form of a particular protein, Carboxy Peptidase E, begins to transform in the tumor. This protein activates genes responsible for secondary growth in the tumor. Early detection of this type of phenomenon would provide another important and powerful weapon for cancer treatment.
setTimeout(function(){
!function(f,b,e,v,n,t,s)
{if(f.fbq)return;n=f.fbq=function(){n.callMethod?
n.callMethod.apply(n,arguments):n.queue.push(arguments)};
if(!f._fbq)f._fbq=n;n.push=n;n.loaded=!0;n.version=’2.0′;
n.queue=[];t=b.createElement(e);t.async=!0;
t.src=v;s=b.getElementsByTagName(e)[0];
s.parentNode.insertBefore(t,s)}(window,document,’script’,
‘https://connect.facebook.net/en_US/fbevents.js’);
fbq(‘init’, ‘836181349842357’);
fbq(‘track’, ‘PageView’);
}, 6000);
/*setTimeout(function(){
(function (d, s, id) {
var js, fjs = d.getElementsByTagName(s)[0];
if (d.getElementById(id)) return;
js = d.createElement(s);
js.id = id;
js.src = “//connect.facebook.net/en_US/sdk.js#xfbml=1&version=v2.11&appId=580305968816694”;
fjs.parentNode.insertBefore(js, fjs);
}(document, ‘script’, ‘facebook-jssdk’));
}, 4000);*/